Collaborative, Human-Centered Approach to Workflow Optimization
Observation and Interview
Accessible Version of Collaborative, Human-Centered Approach to Workflow Optimization Case Study
This is a text-based version of the embedded Canva presentation for screen reader users and others who prefer accessible HTML.
Slide 1: Case Study Title Page
Title: Collaborative, Human-Centered Approach to Workflow Optimization
Author: Sarah Casteel
Case Study Home: View embedded and accessible case study (opens in new tab)
Slide 2: Case Study Introduction
Introduction: Hi, I'm Sarah.
I’m a UX + Human Factors Researcher, software user advocate, systems thinker, and UNC grad (MSIS ‘21).

This case study reviews a six-month service design project with a large government health system.
Slide 3: Agenda
This presentation includes the following topics. Select a topic to jump directly to that section.
Slide 4: Summary
- Primary Objective
- Identify opportunities to improve process and increase Women’s Health critical workflow efficiency.
- Methods
- Mixed Methods Approach
- In-person observation and interview
- Clinical Site 1: October 21–23, 2024
- Clinical Site 2: November 5–7, 2024
- Collaborative cross-functional workshop to share + prioritize findings, create action plans
- Post-workshop user satisfaction survey
- In-person observation and interview
- Mixed Methods Approach
- Outcomes
- Delivered observed current state clinical workflows:
- Within phases of the patient experience.
- With the people, activities, technology, friction, resilience, and workflow variation observed.
- Enabled immediate improvements for end users and influenced medium- and long-term product roadmaps through stakeholder collaboration.
- Delivered observed current state clinical workflows:
Slide 5: Project Snapshot
- Client: Large health system undertaking an Electronic Health Record (EHR) transition
- Timeframe: 26 weeks
- My Role: Lead UX + Human Factors Researcher
- Team: Sarah Casteel (Lead); Supporting Human Factors Researcher; Cross-functional team with five key stakeholder groups
- User Roles:
- Women’s Health Provider (Primary Care Physician, Gynecologist, Physician Assistant)
- Licensed Practical Nurse (LPN)
- Registered Nurse (RN)
- Registration and Scheduling Staff (Reg/Sched)
- Methods: Observation, Interview, Satisfaction Survey, Workflow Analysis, Thematic Analysis
- Techniques: Field Note-Taking, Note Transcription and Cleanup, Open + Axial Coding, Deductive Coding, Current State Workflow Visualization, Barrier + Gap Analysis, Classifying Variations, Remote Workshop
- Tools: Pen + Paper, Clipboard, Mobile Phone + Camera, Microsoft tools (Excel, Word, Outlook, PowerPoint, SharePoint, Teams), Lucidchart, Dropbox, Slack, SurveyMonkey
Slide 6: Objectives
“You can optimize everything and still fail, because you have to optimize for the right things.”
- Identify opportunities to improve process/increase critical Women’s Health clinical workflow efficiency.
- Determine specific opportunities to improve EHR user interface issues that contribute to inefficient workflows.
Slide 7: Engagement
- Hold initial kickoff meeting to ensure client + project team alignment.
- Hold weekly planning meetings between project team, client, and interested stakeholders.
- Email post-meeting summaries including key actions and due dates.
- Maintain regular virtual communication (email, Microsoft Teams) providing key status updates throughout project.
Slide 8: Collaboration Framework
- Prioritize and center the internal client’s goals, including breaking down silos between business units.
- Include interested stakeholders across functions in study planning, data collection, and reporting.
- Align research goals with business goals.
- Link human-centered design research with existing processes and initiatives.
- Stakeholder Business Units
- Core Project Team
- Client
- Human Systems Integration (HSI) Study Execution Team
- HSI Government Partners
- Internal Business Units
- Clinical Teams
- Process Modelers
- Standardization Workstream
- External Business Units
- Software Developer: Technical Teams
- Software Developer: Client Success Teams
- Core Project Team
Slide 9: Study Planning
“Everyone's behavior changes with the context and the circumstances.”
- Hold working meetings that emphasize collaboration with stakeholders including EHR consultants, national workgroup leaders, and clinical teams to ensure cross-functional alignment on goals and findings.
- Take a user-centered, contextual approach by observing users complete clinical and EHR workflows in their typical environments to capture workflows as typically done in their typical context (“work-as-done”).
- Prioritize behavior in context over quicker options like remotely interviewing users about workflows that leaders believe users complete (“work-as-imagined”).
- Work with client and stakeholders to select two clinics for field visits to allow observation of common patterns and workflow variations.
Slide 10: Methods
- Qualitative
- Observe and document EHR users’ in-clinic activities, including actions, interactions with people and technology, tasks, and processes.
- Interview users to identify needs and understand the reasons/motivations behind users’ observed actions.
- Quantitative
- Capture clock time for each observed activity to identify efficient and inefficient workflows.
- Distribute end-of-project satisfaction survey to capture baseline satisfaction with EHR software and site visit project activities.
Slide 11: Data Collection
- Site Selection and Scheduling
- Select sites based on considerations including clinic culture, scheduling constraints, and willingness of clinicians and staff to participate.
- Clinic Observation Visits
- Day 1 Introductions: Observers meet users
- Days 1–3
- Morning and end-of-day meetings with onsite and remote stakeholders
- Observation/shadowing sessions with users
- Post-observation interviews with users
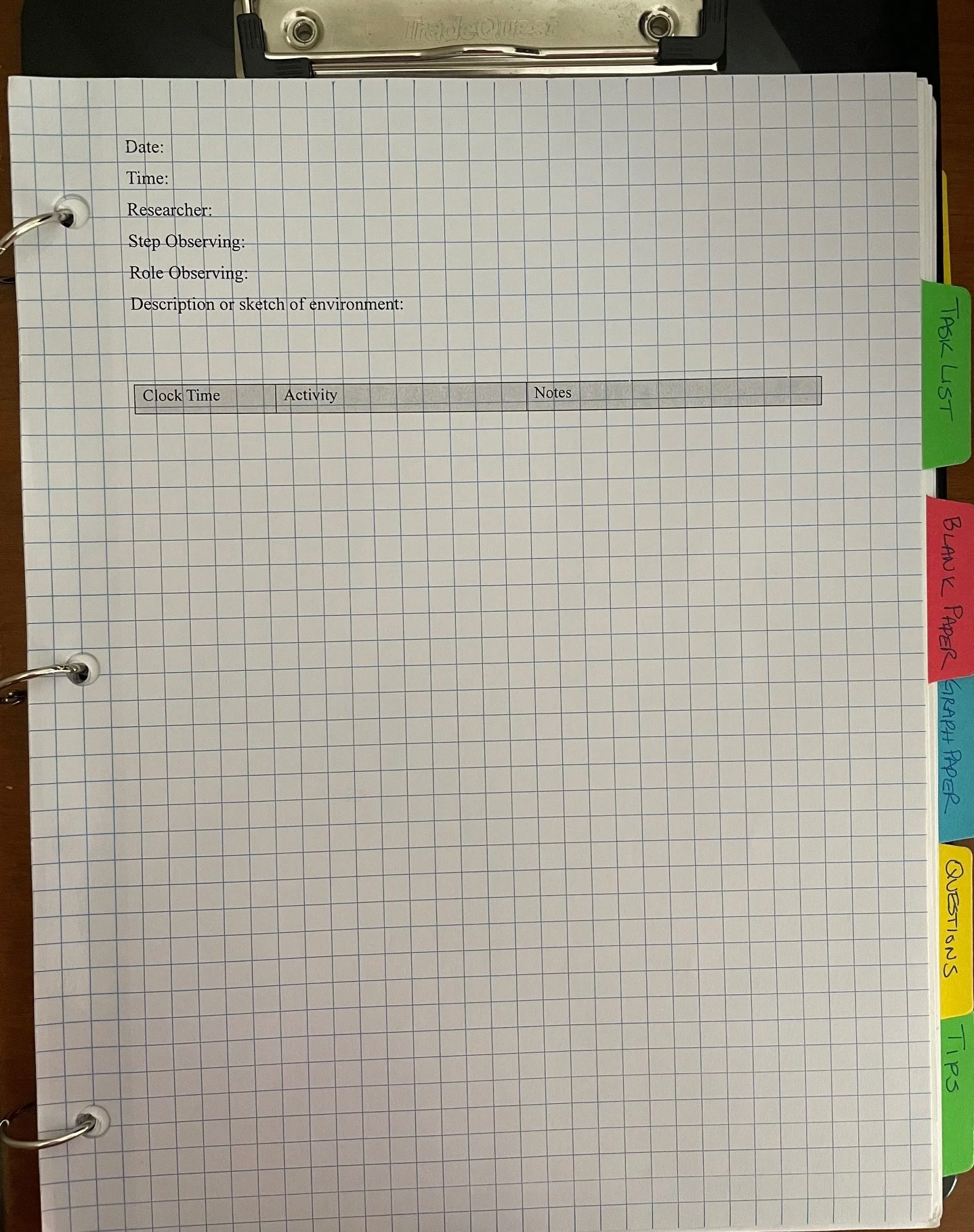
Data collection artifact: Graph paper modified with headings for observation notes.
- End-of-Project Survey
- Distribute satisfaction survey after reporting workshop.
Slide 12: Analysis
- Structured Analysis
- Transcribe data and identify themes, workflow patterns, and workflow variability.
- Workflow Visualization
- Map current state processes and pinpoint pain points and areas of resilience within prioritized clinical workflows.
- Impact Assessment
- Categorize observations, pain points, and workflow variations by impact on workflows and users and link variations to specific sources.
Slide 13: Reporting
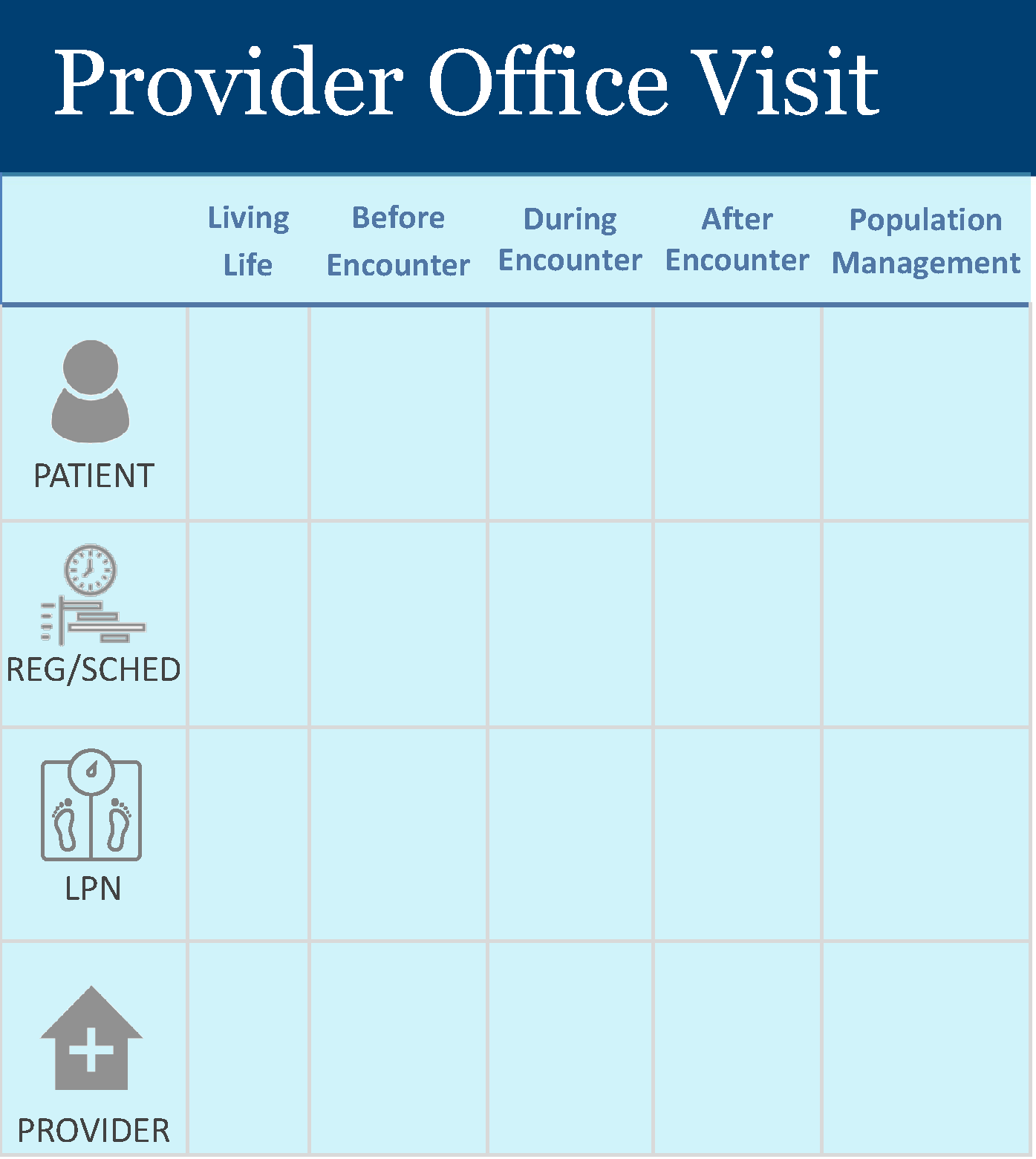
- Create service blueprint visualization for each observed prioritized workflow across phases of the patient experience with the people involved and activities and technology observed.
- Plan and facilitate collaborative remote reporting workshop with key stakeholders and users.
- Interactive discussion of key findings fosters stakeholder engagement, user feedback, and alignment on interpretations of findings and next steps.
- Distribute user satisfaction survey as an activity at the end of the workshop to increase response rate.
Slide 14: Impact
- Immediate and Tactical Value
- Enabled 35+ immediate improvements for users through collaboration during fieldwork, including on-the-spot EHR configuration updates and staff training by EHR consultants.
- Accelerated resolution of longstanding issues, including one critical EHR pain point that had remained unaddressed for 2+ years.
- Actionable Discoveries
- Uncovered 150+ critical pain points across clinician and staff workflows, directly informing a prioritized roadmap of three high-impact EHR configuration changes scheduled for implementation within two months of field visits.
- Informed prioritized roadmap of 50+ additional medium- and long-term opportunities for EHR improvement.
- System Mapping and Shared Understanding
- Synthesized data into eight service blueprints for six roles, offering cross-functional teams a shared, end-to-end view of Women's Health clinical workflows and informing internal workflow standardization.
- Strategic Influence
- Directly shaped leadership’s strategy for a follow-on service-standardization project based on findings, securing stakeholder buy-in for initial scoping.
- Established baseline user satisfaction with EHR technology and site visit activities across two clinics, providing a clear starting point for measuring EHR optimization progress.
Slide 15: Reflection – Study Planning
| Lesson | Revise / Repeat |
|---|---|
| Lesson: Each clinical specialty had its own culture, processes, and perspective on working with outside teams. Early on, some leaders expected the project team to dictate changes to existing processes that worked well for them. |
Revise: Set the right tone early with stakeholders to confirm shared understanding that the project team intends to learn and socialize what’s working well rather than change existing best practices. |
| Lesson: As project complexity increased and more stakeholders joined planning meetings, the increased meeting size seemed to decrease dialogue with site contacts. |
Repeat: Smaller site logistics meeting before second field visit encouraged more open dialogue with key site contacts. Build site-specific logistics meetings into planning 2–3 weeks before field visits. |
Slide 16: Reflection – Data Collection
| Lesson | Revise / Repeat |
|---|---|
| Lesson: The study team coordinated both virtual and onsite observations, which overlapped at the first field visit. Multiple data collection activities confused participants and the study team inadvertently excluded a key stakeholder from virtual activities. |
Revise: Balance the tradeoffs of increased complexity with the impact of complexity on data collection activities and timelines. For example, plan virtual observations for the week before field visits. |
| Lesson: Coordinating field visits with multiple stakeholder groups can and should be done to encourage shared human-centered understanding of clinical and EHR workflows, and multiple groups of observers can be stressful for participants. |
Repeat: Study team completed Day 1 observations with just two observers, allowing time to introduce clinical users to observations without overwhelming them. Balance stakeholder and participant needs by easing participants into Day 1 observations with as few observers as possible. |
Slide 17: Reflection – Data Analysis
| Lesson | Revise / Repeat |
|---|---|
| Lesson: More project complexity resulted in more data in the same amount of time compared to previous project iterations. |
Revise: Balance the tradeoffs of increased complexity with the impact of complexity on data analysis. With complex data, analysis may be at a higher level than stakeholders expect, or project timeline should expand to allow for deeper analysis. Communicate these expectations to stakeholders. |
| Lesson: Qualitative analysis of observation and interview data is complex and requires both clear direction to and collaboration with analysis team. |
Repeat: Provide analysis team with a clear analysis plan and be ready for questions. Work through data reconciliation with team at regular intervals. |
Slide 18: Reflection – Reporting
| Lesson | Revise / Repeat |
|---|---|
|
Lesson: Technology constraints like limited visibility into active Microsoft Teams polls present challenges during remote workshops. |
Revise: Run through all aspects of technology logistics, particularly for interactive activities, with the meeting owner before remote workshops. Always have an activity backup plan in the event that technology fails. Communicate these expectations to stakeholders. |
|
Lesson: An informal icebreaker activity that tied into study findings increased workshop participation and engagement. |
Repeat: Incorporate intentional, well-planned icebreaker activities into remote workshops. |
Slide 19: Reflection – Momentum and Follow-up
| Lesson | Revise |
|---|---|
| Contracts can be terminated at any time. The contract supporting this work was terminated early amid efforts to better quantify the impact of the changes made as a result of this work on users. | Where possible, incorporate existing baseline measures and/or telemetry into study preparation and tie research outcomes to these baselines during analysis and reporting. |
Slide 20: Presented at the Human Factors and Ergonomics Society (HFES) International Symposium on Human Factors and Ergonomics in Health Care
I presented this collaborative, impactful work as a poster at the March 31, 2025 HFES International Symposium on Human Factors and Ergonomics in Health Care in Toronto, Canada, which hosted 735 attendees.

Slide 21: Thank You
Case Study by Sarah Casteel | Health Service Design | 2025